
Blunt Eye Injury
Case Study: Blunt Eye Injury
Dr Daniel Chiu
A 56 yo healthy male reported left eye blunt injury, hit by tennis ball some 10 years ago. He was referred for assessment of blurred vision Left for last 2 years for possible epiretinal membrane.He visited an ophthalmologist 5 years ago and patient received laser peripheral iridotomy prophylaxis, and had not been reviewed since.
On examination:
- Right unaided vision 6/6
- Left unaided vision 6/60 with aided vision 6/24 with -1.50D
- Left anterior chamber more shallow than Right
What next?

What clinical parameter would you want to know next?
IOP: Right IOP 15, Left IOP 6;
lens status: Right clear lens, Left 1+ nuclear cataract
What is the next clinical examination you would want to perform?
Fundoscopy dilated preferably. You found the optic disc cupping are symmetrical at 0.3 each eye. Left macular reflex “odd”
What special investigation you may want to perform or request?
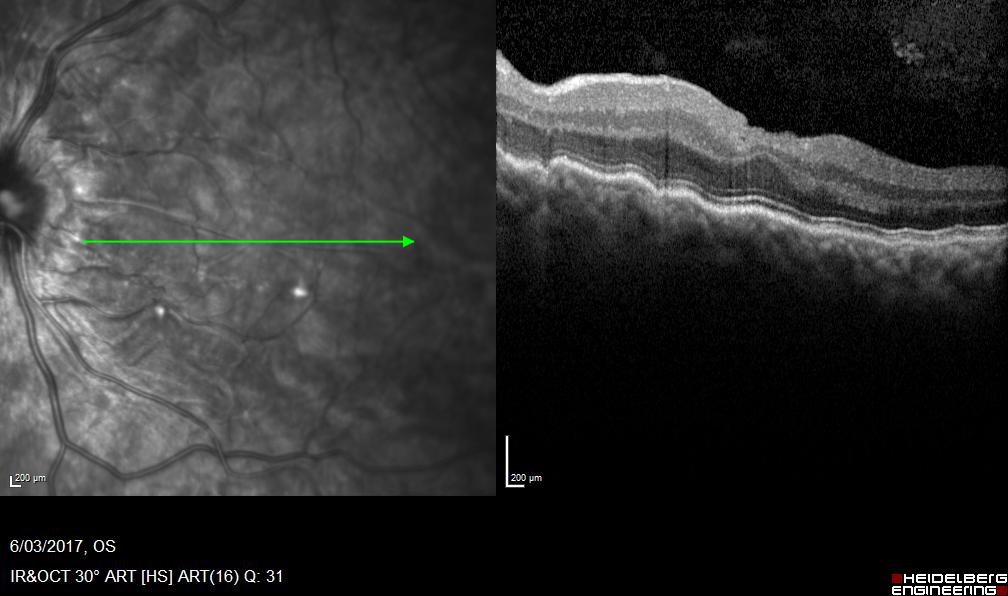
OCT of maculae. See Fig 1 & 2

What is your OCT interpretation?
Left full thickness corrugation of neuroretina, RP and choroid. Preservation of internal retinal layered architecture, minimal increase of retinal thickness, lack of any visible epiretinal membrane on cross-section
What is your working diagnosis and what may be the underlying cause?
Left hypotonus maculopathy. Possible cyclodialysis cleft after blunt injury, with or without some lens instability and forward movement explaining shallow anterior chamber only in Left eye. Previous laser iridotomy for shallow anterior chamber is neither helpful nor causative.
How would you confirm your diagnosis?
Contact gonioscopy on undilated pupil looking for dialysis “cleft” or gap between iris root and scleral spur. If anterior part of the gap is visibly bare sclera deep into the cleft, it means there is a detachment or disinsertion of the ciliary body from the sclera and there is an much increased uveoscleral outflow of aqueous into the suprachoroidal space, leading to hypotony.
Diagnosis
This gentleman was found to a cyclodialysis cleft of one clock hour size nasally on gonioscopy and is thus scheduled for surgical repair, attempting to reverse the hypotonus maculopathy.
Lesson: not all corrugated macular surface on examination or OCT with reduced vision is epiretinal membrane.



