Rapid Resolution of Unilateral Haemorrhagic Retinopathy in a Young Patient
Case Study: Rapid Resolution of Unilateral Haemorrhagic Retinopathy in a Young Patient
Dr Daniel Chiu
33 yo ICU nurse on maternity leave, recently gave birth to her first born 5 months ago.
She presented with one week history of sudden onset of flickering left temporal vision and
discomfort with light changes, finding it slow in adjusting to changing lighting condition in her left
eye.
She suffered from gestational diabetes (now resolved) and has family history of diabetes.
Prior to the onset of her vision problem, she exercised heavily with a long game of tennis on a
very hot day. She is fully breast-feeding as well.
On examination, RVA 6/6 LVA 6/6 with low myopic correction. IOP 9 mmHg each eye.
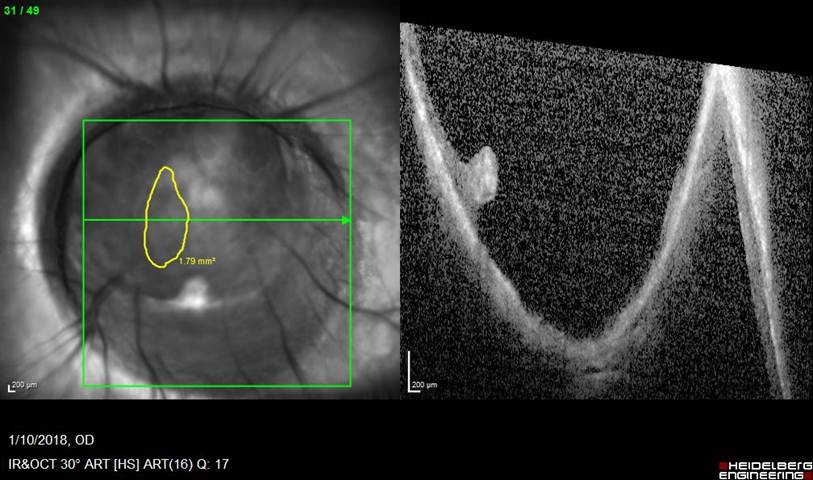
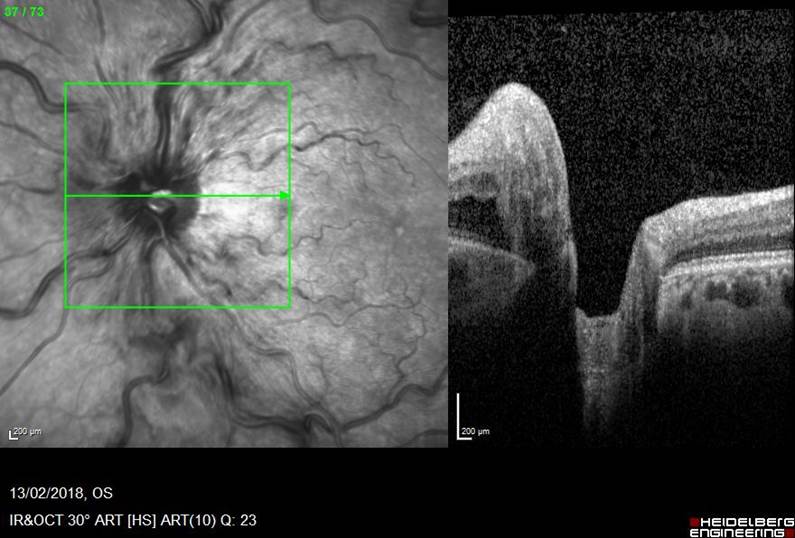
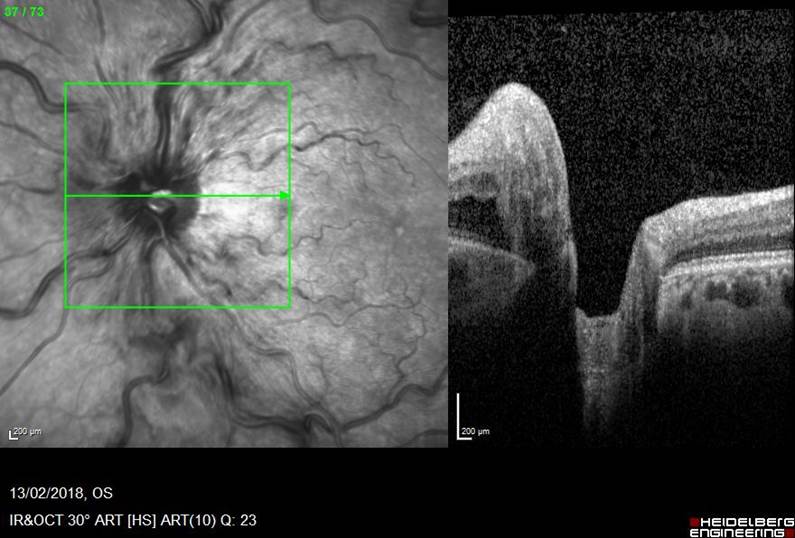
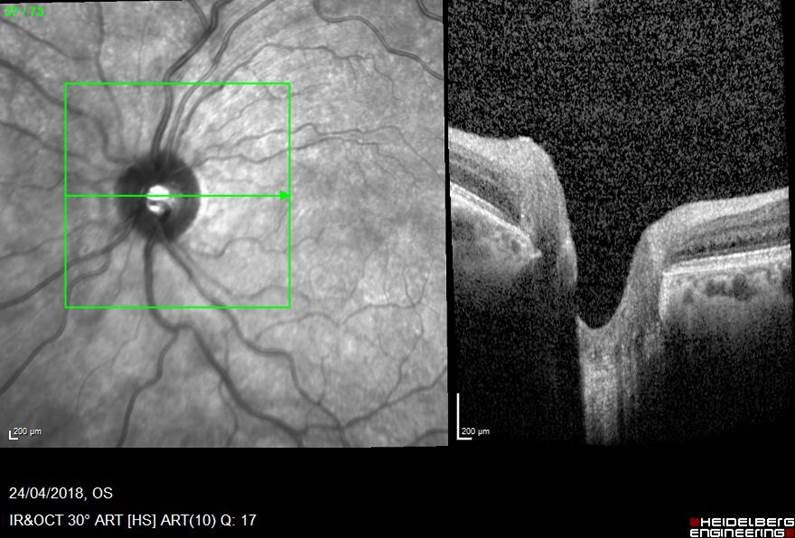
Left Fundal (red-free SLO image) and macular OCT. Right side entirely normal.
Rank the likely diagnoses from the following in descending order:
- Diabetic retinopathy
- Diabetic papillitis
- Central retinal vein occlusion
- Papilloedema
- Hypertensive retinopathy
Click for answer.
Based on a unilateral finding of swollen disc, engorged tortuous vein, nerve fiber layer
haemorrhage and lack of macular oedema, without any sign of microaneurysm visible in the
photo, the ranking of likely diagnoses is:
- Central retinal vein occlusion (non-ischaemic, mild)
- Hypertensive retinopathy (should be at least bilateral but can be asymmetric and would
be of at leave grade 3-4) - Diabetic papillitis (a misnomer but can be seen in young diabetic whose diabetic control
is tightening rapidly) - Diabetic retinopathy (should have some other sign of DR and bilateral)
- Papilloedema (rare to be unilateral and unlikely to have vascular changes unless very
severe and chronic)
What is the most critical clinical or imaging finding that will support your most likely diagnosis you listed in question 1, above?
Click for answer.
This answer of course depends on your answer in Q1.
For central retinal vein occlusion, the most reliable sign is elevated closing venous pressure to a level at least equal or above the systolic perfusion pressure of the central retinal artery. This test is achieved by using a 90D or macular fundus lens examining the disc and at the same time, digitally compressed the globe to look for CRV collapsing before or after the CRA starts winkling. Engorged tortuous retinal vein is also a common sign but may not be evident in some older patients especially if associated with significant glaucomatous cupping. Scattered retinal haemorrhage in all 4 fundal quadrant is also often present to a varying degree. Macular oedema on OCT can also be absent in mild case.
What would be an appropriate follow-up management based on your decision in question 1?
- Suggesting anti-VEGF injection and refer to an ophthalmologist to perform it
- Write to GP and suggest an MRI
- Write to GP and recommend further blood tests
- Close observation and refer to ophthalmologist for opinion
Click for answer.
Option 4 would be the most appropriate. Despite much hype on anti-VEGF treatment, it has no role in mild CRVO without any macular oedema, even if there are clear cut scattered haemorrhage. There is no proof in its role in altering the progression or regression of CRVO natural history without macular oedema. Clinically this patient either has a n incomplete occlusion or an occlusion of the central vein that rapidly recanalized. This often can be the case in a young patient with CRVO. Close observation is recommended to following up on further re-occlusion event or development of macular oedema. Once again, preemptive anti-VEGF injection has no proven role in avoiding macular oedema or re-occlusion.
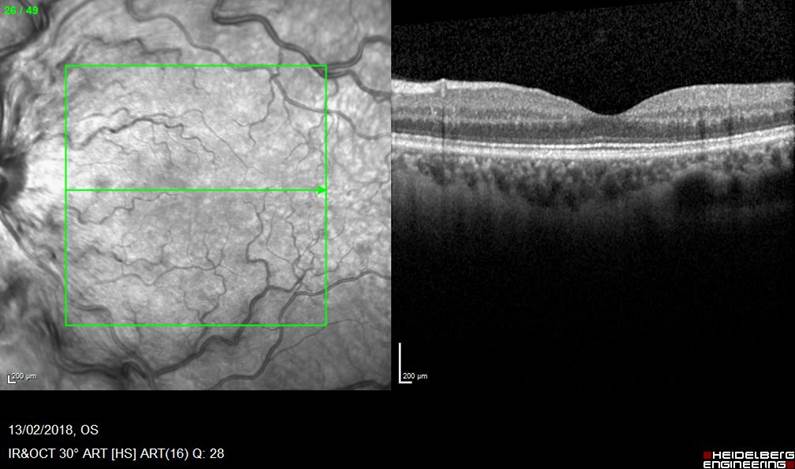
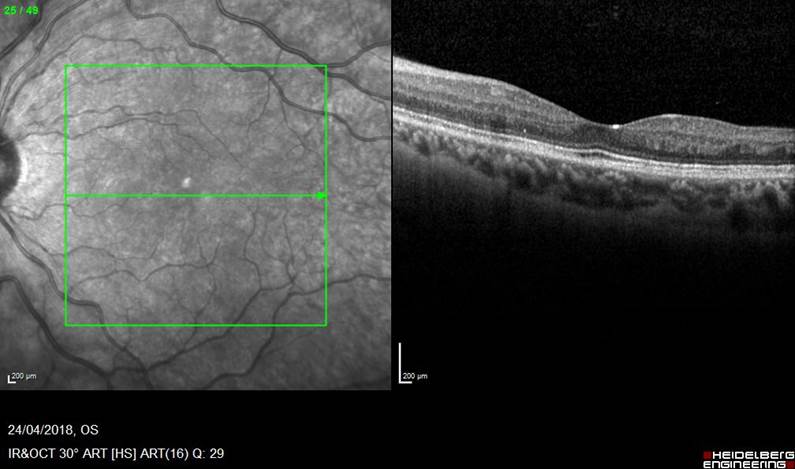
This is her fundal image after 6 weeks after visiting a retinal specialist. What has happened? What do you think may be the cause of her presenting problem?
Click for answer.
Clearly recanalisation occured and her fundal signs all resolved without any intervention. Systemic hypertension and diabetes as a risk factor should be excluded by referring to GP, but blood tests for pro-thrombotic screening is often unhelpful unless on history there was other thrombotic event or family history. Isolated single incidence of CRVO would not lead to long term prophylactic use of anti-coagulation therapy.
In this particular case, I hypothesize the precipitating event for her CRVO could well be dehydration with heavy exercise on a hot day without adequate fluid intake and she also had been full breastfeeding her 5 month old before. Very likely other unknown systemic and localised ocular factors are involved in her case, but in the absence of other common reversible and preventable risk factor, one would have to take dehydration as a preventable risk and I did
encouraged her to ensure adequate fluid intake, especially with breastfeeding.
So largely this patient has been very lucky and her CRVO fully resolved.