A Case of Hypertensive Uveitis
Case Study: Hypertensive Uveitis
Dr Janice Thean
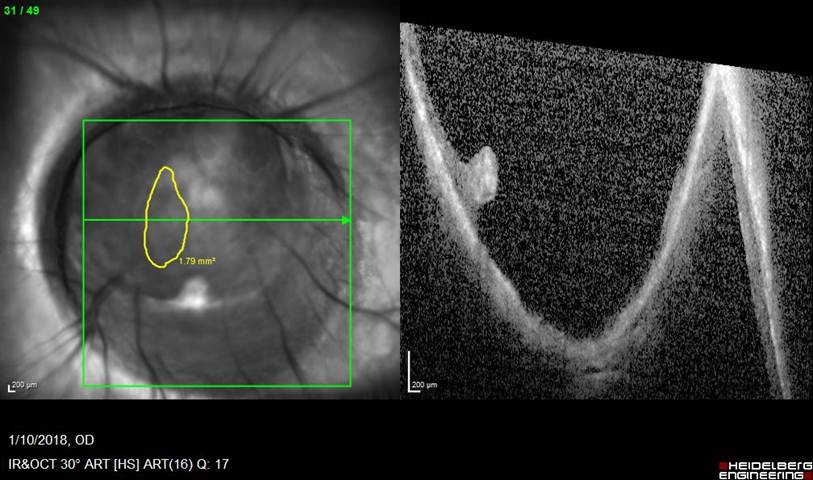
A 74 year old man presented with a 3 week history of gradual blurring of his left vision. There was associated mild ocular redness and Chlorsig drops from his GP did not resolve it. VA on presentation was 6/36, IOP was 45 and the eye looked like this
What are the likely differential diagnoses?
Click for answer.
- Herpetic uveitis
- Posner-Schlossman syndromeFuch’s
- Heterochromic iridocyclitis
What other history would you need to get?
Click for answer.
-
Previous similar episodes?
-
Previous history of shingles?
-
Previous history of cold sores?
-
Previous history of HLA-B27 related conditions?
What other signs would you need to look for?
Click for answer.
-
corneal sensation
-
presence of dendrites
-
dilated examination to rule out vitritis and retinitis
-
is the other eye involved?
-
any signs of iris atrophy?
-
presence of peripheral anterior synechiae and posterior synechiae
What treatment would you start him on?
Click for answer.
Intensive topical steroids, cycloplegics and an IOP lowering agent.
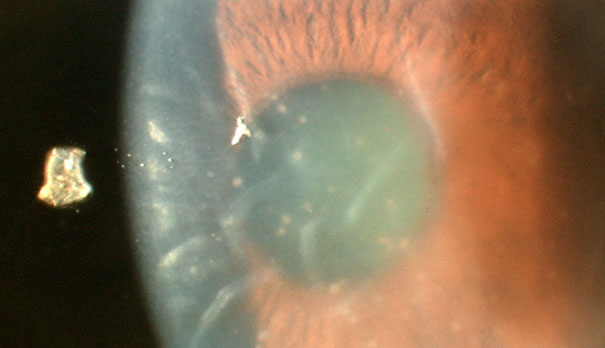
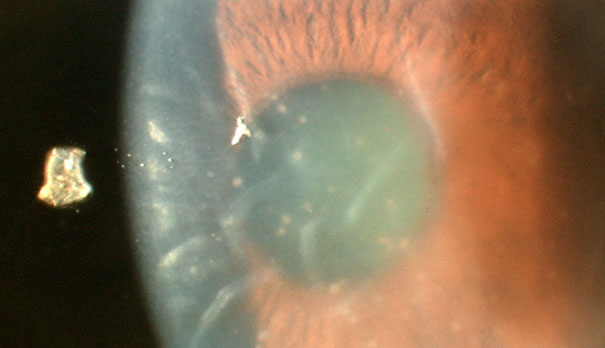
At his review at 1 week, VA had improved to 6/12, IOP was 15. However, there was residual anterior chamber inflammation and the eye now looked like this:

What would you need to do now?
Click for answer.
It looks like a dendritic ulcer. So the most likely diagnosis is herpetic uveitis. Aciclovir eye ointment was added to the current regimen of treatment.
Discussion
The development of acute anterior uveitis is usually associated with a lowering of intraocular pressure, as inflammation of the ciliary body results in a decrease in aqueous production while aqueous outflow is enhanced by increased uveoscleral outflow. When faced with a case of acute anterior uveitis with increased intraocular pressure, one must consider an infective cause.
By far, the most common cause of hypertensive uveitis is herpetic in nature (HSV, VZV, CMV). All these are typically unilateral with HSV and VZV associated with iris stromal defects. The presence of a dendrite or disciform keratitis also helps with the diagnosis. Most of the time, a detailed history and careful examination is usually enough to achieve a correct diagnosis. CMV uveitis unfortunately, often requires an AC tap for PCR for correct diagnosis. Other infective causes could include Toxoplasmosis which often will have associated vitritis and retinal lesions.