What’s that in the Angle?
Case Study: Neovascular Glaucoma
Dr Janice Thean
Presentation 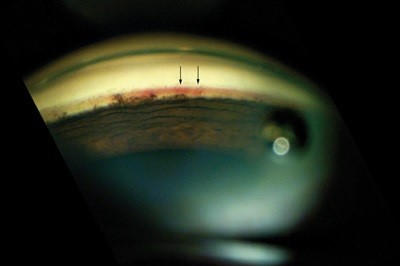
A 59 y.o diabetic truck driver went for his usual eye check for license renewal. He was found to have an IOP of 50 in the left eye, right 16 and a left visual field defect was found on subsequent VF testing. Patient was asymptomatic, in particular had not experienced any visual symptoms. He had a RVA of 6/6 and 6/9 on the left. Significant past history consists of quiescent right PDR and moderate left NPDR and bilateral cataract extraction.
Clinical findings
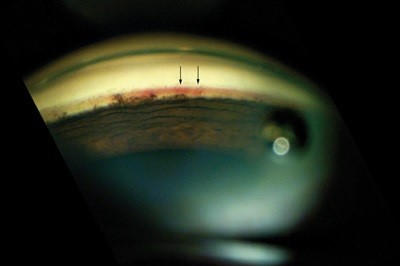
Anterior segment examination showed no signs of obvious signs of rubeosis, PXF or PDS. Anterior chamber was quiet, in particular no signs of a flare. Gonioscopy showed an open angle with no signs of PAS but areas of fine tufts of blood vessels in the angle.
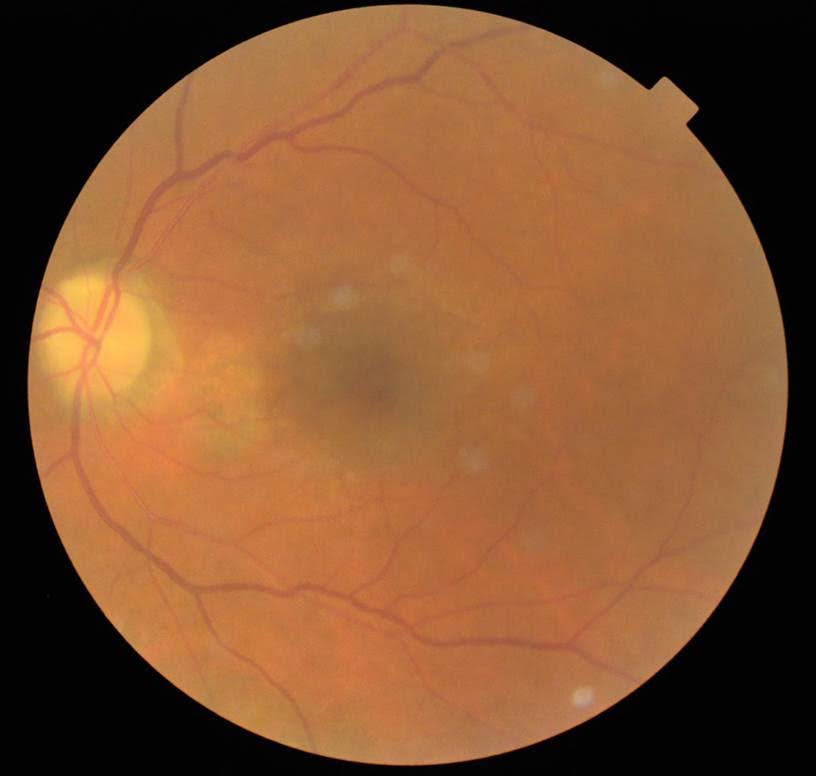
Fundus examination of the right eye showed full PRP. Left eye showed minimal PRP done in the past with some macula laser. There was an area of NVD inferior to the optic disc.
The diagnosis for this patient is neovascular glaucoma due to underlying retinal ischemia from diabetes. This case illustrates the importance of doing routine gonioscopy as this was the only thing that provided clues to what the cause of the raised IOP was.
Treatment consisted of pressure lowering medications (Diamox, Alphagan, Azopt and Timolol), in addition to prednefrin forte qid. The patient was brought back a week later for anti-VEGF injection (Avastin was given in this case) when the IOP had normalized.
Long term treatment for this patient will include fill in PRP to reduce the ischemic drive and possibly further anti-VEGF treatments.
Discussion
Neovascular glaucoma (NVG) is a severe form of secondary glaucoma characterized by proliferation of fibrovascular tissue in the anterior chamber angle. The patient can present either with a secondary open angle or secondary closed angle mechanism depending on the extent of neovascularization. When new blood vessels appear within the anterior chamber angle, aqueous outflow can be compromised with extension of these new vessels across the scleral spur and subsequent obstruction of the trabecular meshwork. The new blood vessels are usually accompanied by a fibrous membrane, and contraction of this membrane results in formation of peripheral anterior synechiae and progressive angle closure.
The main predisposing factor for this condition is underlying retinal ischemia. Main causes include retinal vein occlusion and diabetic retinopathy. Other causes include carotid occlusive disease, CRAO, ocular tumours and previous history of irradiation.
NVG is a potentially devastating glaucoma, where delayed diagnosis or poor management can result in complete loss of vision or, quite possibly, loss of the globe itself. Early diagnosis of the disease, followed by immediate and aggressive treatment, is imperative.
Management
In managing NVG, it is essential to treat both the elevated intraocular pressure (IOP) and the underlying cause of the disease.
Adequate treatment of retinal ischemia with PRP is essential in reducing the stimulus for neovascularization of the anterior segment, which may prevent the need for additional surgery. Treatment of underlying systemic disease may improve neovascularization of the iris, as is the case with endarterectomy for carotid occlusive disease and ocular ischemia. The advent of anti-VEGF agents has lead to their use in the form of intravitreal injections prior to PRP. The duration of suppression of iris and angle neovascularization lasts approximately 3-6 wks with anti-VEGF injections, thereby creating a window of opportunity to allow adequate PRP to be carried out.