To Jab or to Zap?
Case Study: Diabetic Maculopathy
Dr Daniel Chiu
Presentation
This case highlights some of the management issue of diabetic retinopathy.
- 54 yo male
- First presentation for diabetic eye check as newly diagnosed Type 2 Diabetic in 2015.
- Initial VA 6/6 bilaterally with moderate NPDR.
- Followed up 6 monthly until mid 2016.
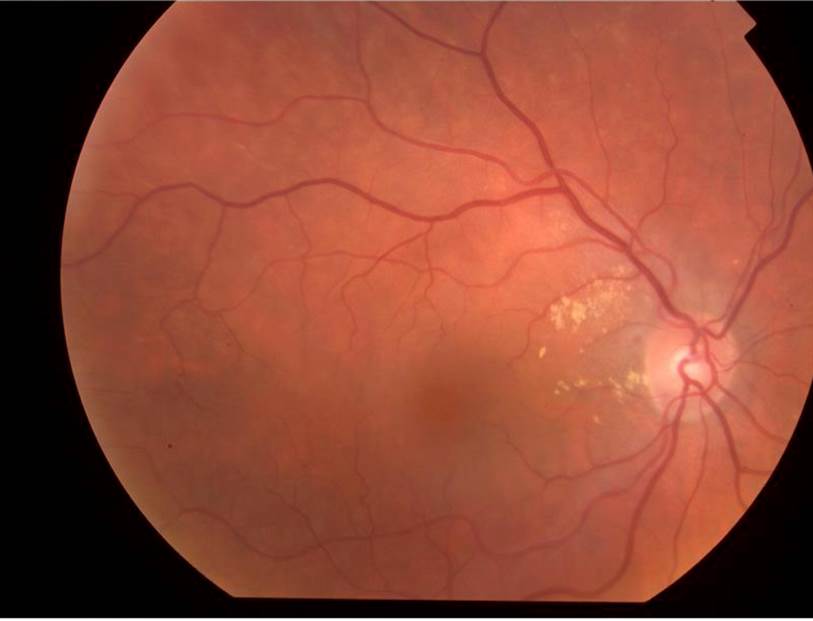
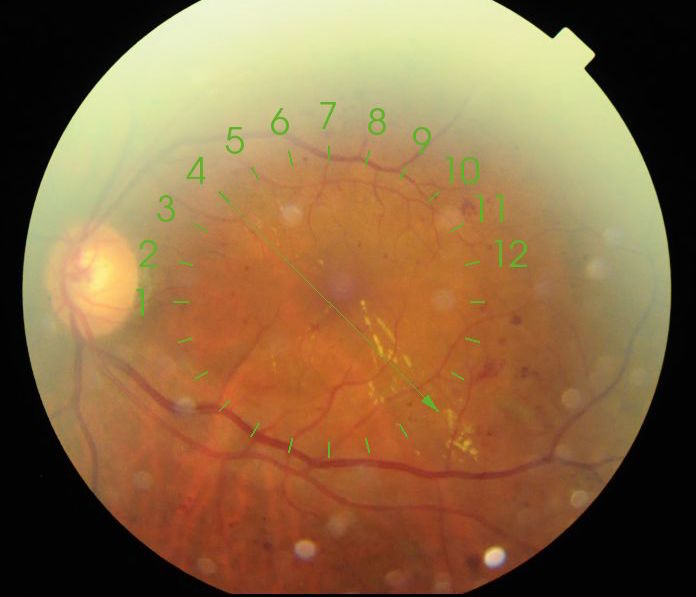 Figure 1. Left fundus Colour 2016 Left VA 6/6
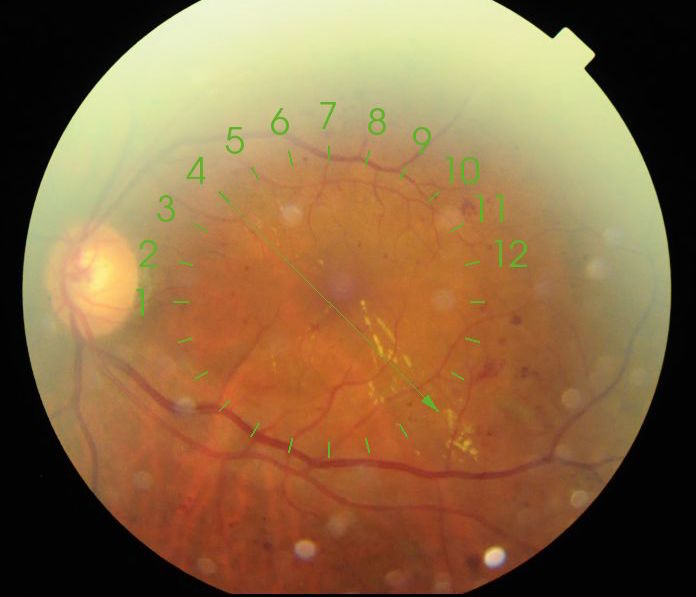
Figure 1. Left fundus Colour 2016 Left VA 6/6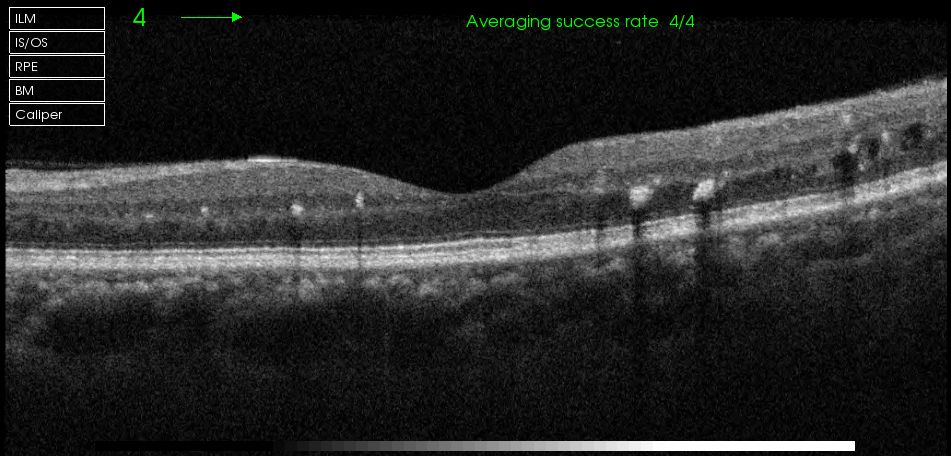 Figure 2. OCT Left macula 2016
Figure 2. OCT Left macula 2016What is the vision threatening finding?
Main findings at his stage in his Left eye is moderate NPDR with lots of small haemorrhages and microaneurysms in the temporal posterior pole. Most concerning is the streak of lipid exudates arranged radially at 4 o’clock tracking towards fovea. Clinically it strongly supports the diagnosis of Clinically Significant Macular Oedema (CSME) as described in the Early Treatment Diabetic Retinopathy Study (ETDRS).
What is the relevant good finding? Any concern?
The good finding is that fovea centre is free from oedema but the concern is that there are numerous hyepr-reflective foci representing intraretinal lipid deposits and some small intraretinal cysts temporally.
What is the treatment option, if any? (A) No intervention, continue observe (B) Regular anti-VEGF injection as per published randomised control trials and protocols (C) Macular laser as per ETDRS findings (D) Intravitreal steroid injection
Both A and C are acceptable options. Choice between the two depends on patient aversion to laser treatment, his attendance record indicating whether he is willing to be followed up closely and his systemic risk factors control such as diabetes and blood pressure. I chose macular laser treatment by applying highly focussed laser spot directly to the numerous small microaneurysms which are the leaking source of fluid and lipid exudates. Careful treatment should avoid deeper laser burn to the RPE layer if possible, and of course avoiding treatment very close to the foveal region.
Options B and C are not ideal. Anti-VEGF is only proven to be valuable in centre-involving diabetic macular oedema (DME) where the fovea centre is involved in the retinal thickening. In my opinion, even if one were to use anti-VEGF such as Lucentis or Eylea, multiple monthly injections would be required to help resolving the lipid exudates in this otherwise healthy eye with 6/6 vision. Equal precaution should be given to intravitreal steroid injection especially in phakic eye.
Fast forward to 2017 now. RVA 6/6 LVA 6/5. His diabetes control is improved.

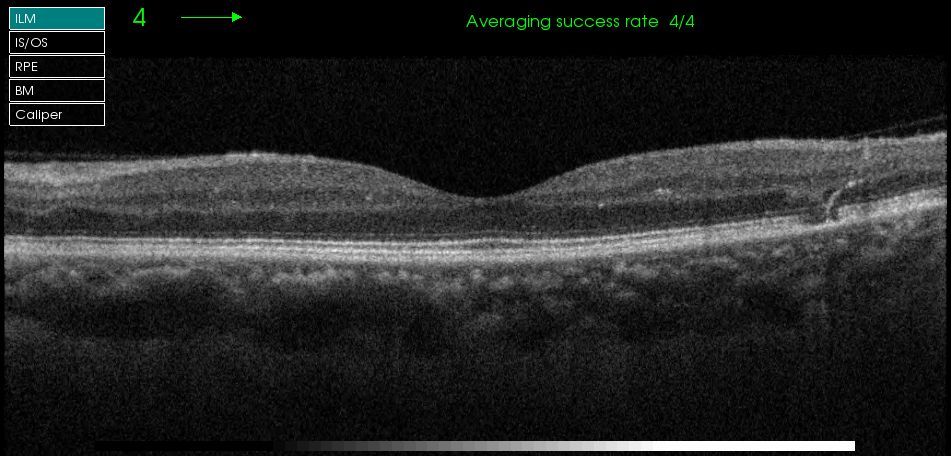 Figure 3. Left fundus Colour and macula OCT 2017
Figure 3. Left fundus Colour and macula OCT 2017
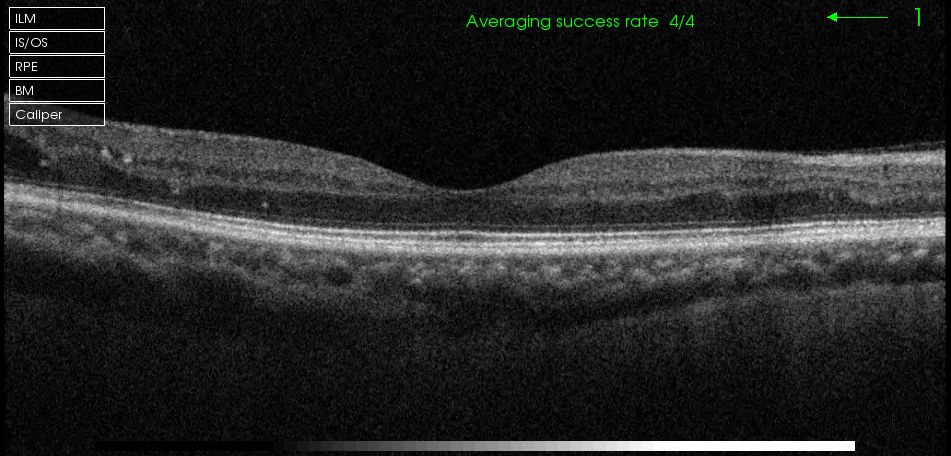 Figure 4. Right fundus Colour and macula OCT 2017
Figure 4. Right fundus Colour and macula OCT 2017Now Lucentis and Eylea have many longer term RCT proven evidence for treatment of diabetic macular oedema, what do you recommend? (A) No intervention, continue observe (B) Regular anti-VEGF injection as per published randomised control trials and protocols (C) Macular laser as per ETDRS findings (D) Intravitreal steroid injection
One can see in Figure 3 that all lipid exudates are gone and OCT showed resolution of intraretinal deposit and cystic changes. One can see a focal area of outer retinal changes possibly related to a small focal laser treatment spot. For the Right eye, the findings is earlier but similar to the left in 2016. There is a faint streak of early lipid at 10 o’clock in the macular region centrally and a small ring of circinate lipid exudate at 9 o’clock just outside the OCT raster. Once again, options B and D are not appropriate for the same reason like the left eye in 2016. Given good response and visual outcome in his Left eye from previous laser treatment, the patient would like have the same for the right to prevent more lipid deposits and a situation where early CSME becoming centre-involving DME. Then the only viable choice remaining to stabilise or improve vision will be multiple anti-VEGF injection monthly for possibly 6 months.
He is booked for focal macular laser treatment targeting all the small microaneurysms in the temporal macula.
Summary
To deliver successful and safe macular laser treatment requires a lot of training, precision and skill. The confidence of newer generation of medical retinal specialists is diminishing because of lack of exposure during training as well as sometimes the ease of delivering anti-VEGF injections as the only treatment option by waiting until macular oedema and lipid deposit involving the fovea centre so that the patient is eligible for treatment under current clinical guideline. A well proven safe laser treatment in trained hands is under utilised.
This is my reflection on this fairly straightforward case of diabetic macular oedema management.