Headaches and Ptosis
Case Study: Headaches and Ptosis
Dr Charles Su
Here is a situation to consider. It is neither a spot diagnosis nor a test of knowledge. The aim of this exercise is to cast eye findings in a certain light by thinking through possibilities and considering what types of evidence are more helpful than others. I suggest that you use the questions to think through the situation and to clarify your own thoughts rather than see them as right or wrong propositions (although they do have answers!)
A 36 year old male family friend telephones you at 3pm on a Thursday complaining of headache and a droopy R eyelid. It came on quickly over 1 hour, 2 days ago, and he thinks that it might be getting worse, and wonders if you can see him before he goes to work the following morning in your clinic. You are in the supermarket doing grocery shopping.
What type of condition do you think that you are facing ?
- a neurological emergency
- a neurological condition that will take time to investigate eg myasthenia gravis
- orbital cellulitis
- probable iritis
- migraine
If your mobile phone was running low on battery power, which question would you ask first?
- have you had this before?
- can you see normally out of the right eye?
- how bad is the headache?
- did you have any double vision?
Which of the following would be unhelpful ?
- asking him to send you a selfie.
- telling him to go to the nearest emergency department
- arranging to get into the office 15 minutes earlier tomorrow in order to see him.
Discussion
Although ophthalmologists might be guilty of cutting themselves off from general medicine, the eye is often a rich source of evidence for things happening elsewhere.
I hope that thinking through the questions will reinforce to you the view that eye and periocular signs are frequently neurological signs.
Hence your friend has a sudden onset of a neurologic deficit combined with headache. The safest attitude to take is to consider this a neurological emergency.
Neither the severity or lack of it, of the headache, nor whether he has had it before, is going to disprove your hypothesis that it is a neurologic emergency, but another neurologic deficit, if present, would raise your threat alert level significantly. Visual acuity could be hard to evaluate, but the presence of diplopia would mean that you are dealing with a cluster of neurologic signs.
A selfie is often useful to verify that a patient’s description matches what is physically present, although in this case your friend’s report is hardly equivocal. There is no doubt, however, that an acute neurologic deficit combined with a headache in a young person could be a rapidly evolving intracranial process, and this is not something which can wait for an evaluation in the morning.
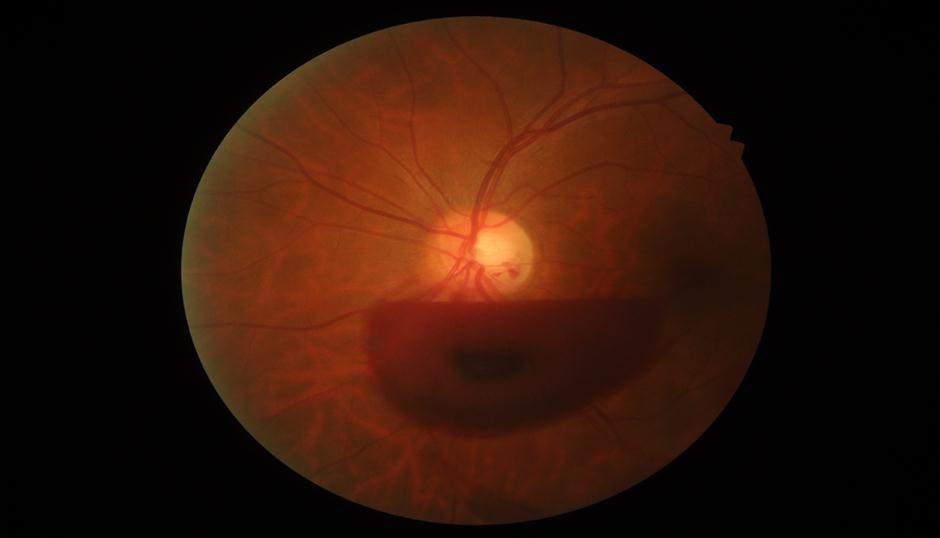
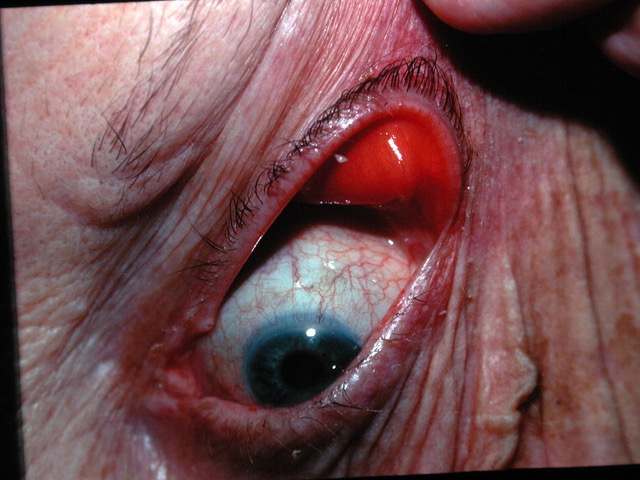
The condition which in this case would explain all the findings, and which cannot be ruled out other than by further immediate clinical evaluation and emergency imaging, is that of an enlarging posterior communicating artery aneurysm, which might be threatening to rupture.
This artery runs parallel to the oculomotor nerve, the third cranial nerve.
Whilst testing eye movements and pupils will be essential parts of defining this friend’s process, it is important to remember the broad category of neurologic emergency which such a situation falls into, and not require signs to be absolutely typical before taking urgent action. After all, it is rare to have “full hands” and partial oculomotor deficits can be difficult to fully characterise for non specialists. Even the headache and acute ptosis alone are enough to consider this an emergency until proven otherwise. Certainly atypical migraine and myasthenia cannot be ruled out with the information you have so far, but they are much less urgent to look into, and not immediately potentially life threatening.